

“The mice have relatively mild disease, which allows us to ask exactly the question I was wondering,” Monje tells The Scientist.
In the study, Monje and her colleagues used a mouse model for mild SARS-CoV-2 infections developed at the lab of Yale School of Medicine biologist and study coauthor Akiko Iwasaki as well as brain tissue samples taken from people who had COVID-19 when they died to demonstrate that mild infections can trigger inflammation in the brain. But because her lab doesn’t study viral infections, she had no way to test her hypothesis until other researchers created the appropriate models. See “ Mechanisms of Long COVID Remain Unknown but Data Are Rolling In”Īs far back as March 2020, Monje feared that cytokine storms caused by the immune response to SARS-CoV-2 would cause the same neuroinflammation and symptoms associated with CRCI, she tells The Scientist. “It is neuroinflammation that happens even in the absence of any central nervous system infection,” Monje tells The Scientist.

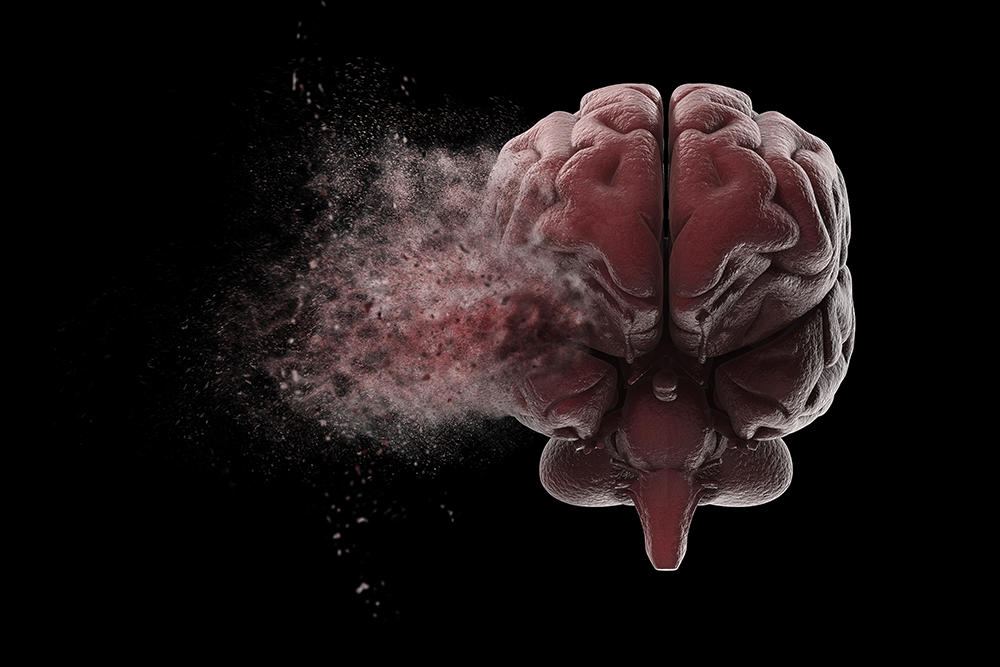
On top of that, the preprint shows that the neuroinflammation pathway can be triggered even without the coronavirus infecting a single brain cell. However, a preprint shared online on January 10 suggests that even mild SARS-CoV-2 infections may lead to long-term neurological symptoms associated with long COVID such as cognitive impairment and difficulties with attention and memory, a suite of symptoms often lumped together as “brain fog.” In the study, which has not yet been peer-reviewed, scientists led by Stanford University neurologist Michelle Monje identified a pathway in COVID-19–infected mice and humans that almost perfectly matches the inflammation thought to cause chemotherapy-related cognitive impairment (CRCI), also known as “chemo fog,” following cancer treatments. Evidence for specific risk factors such as diabetes and the presence of autoantibodies is starting to emerge, but throughout the pandemic, one assumption has been that an important indicator of whether a COVID-19 survivor is likely to develop long COVID is the severity of their acute illness. If it’s attention that’s related to exhaustion, for example, she is going to recommend improved sleep hygiene and stress-reducing measures.As the coronavirus pandemic continues, scientists are racing to understand the underlying causes and implications of long COVID, the umbrella term for symptoms that persist for at least 12 weeks but often last even longer and affect roughly 30 percent of individuals who contract COVID-19. When Madathil determines where the problem happens, she can provide tailored solutions to help. One first has to pay attention, then encode that information, then store it and finally retrieve it. “I'm going to try to break down the steps to memory formation and take a magnifying glass to each of those steps and see where the breakdown is.” “When we look at memory issues as rehabilitation specialists we have to figure out where the breakdown is occurring,” Madathil said. Often a patient’s goals drive the treatments. Cognitive therapists, who are often neuropsychologists, try to determine where the problem starts through a thorough assessment. “Your PCP can take it from there and start targeting a plan to manage some of those issues.” What’s cognitive therapy?įor people who still feel as if medication and behavior changes aren’t improving their thinking, cognitive therapy can help. “You can go to your PCP and say, ‘I’ve been journaling … These are the patterns I have noticed,’” Madathil said. It also helps direct more specific conversations with doctors. That can really help people prioritize healthy behaviors to try to improve their cognition. Sometimes people might realize that on days they sleep poorly they also have more trouble thinking. “Monitor your symptoms by writing them down and keeping a daily journal,” she told TODAY.


 0 kommentar(er)
0 kommentar(er)
